Society

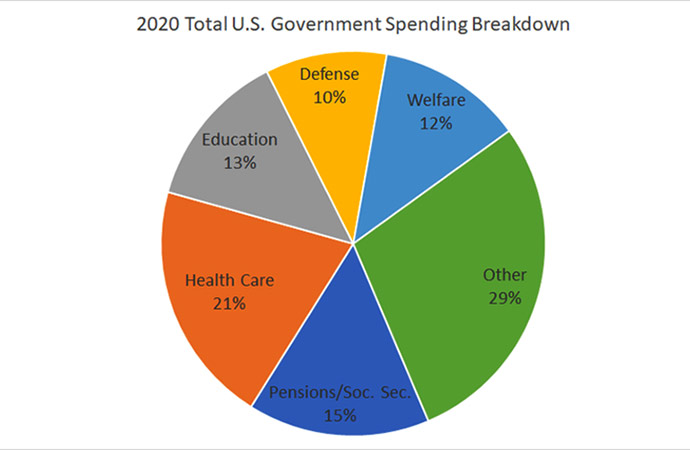
In a country where public sector contribution to healthcare is just 23 percent and people have to bear 67 percent of healthcare expenditure from out-of-pocket (other actors like NGOs shouldering the remaining 10 percent), rise of private sector healthcare service providers should have been well-perceived. But that's not exactly the case here in Bangladesh. A lack of trust and lax monitoring made the otherwise welcome rise in private medicare service look like more a quantity rather than quality. When Bangladesh's public sector appears as one of the world's lowest investor in healthcare, the least it can do is ensure a proper watch over the private sector to ensure people get the right medicare in exchange of a huge money usually they spent to buy the service from private hospitals, clinics and diagnostic centres.
Recent death of a three-year old child due to alleged wrong treatment and negligence at a private health facility in the port city Chattogram prompted our health authorities to conduct drives at private hospitals and clinics. They found out that things were not working in accordance to rules and regulations laid out by the Directorate General of Health Services (DGHS) at many of the private health facilities. What should have been part of a proactive measure - routine monitoring and preventive detection by concerned health authorities, is being unearthed now as a reactive measure. Upon investigation, a DGHS probe body has found 11 irregularities of Max Hospital where the three-year old child Raifa Khan met a tragic end of her life. The hospital authorities did not renew its license in 2017-18. There was no list of specialist doctors, though the hospital claimed it to be a specialized one. There was no detailed information of pathologists who prepared test reports. The hospital in question didn't issue appointment letters to doctors, nurses, cleaners and other employees.
It took life of a kid to jerk DGHS and make it go for some reactive measures i.e. conducting drives and fining the non-compliant hospitals and clinics. But had DGHS played its mandated role in the first place then there should have been no existence of any private hospitals/clinics/diagnostic centers with so many regulations being flouted. It only reflects that somewhere some people are not doing their jobs properly. The sector experts have cautioned many a time on quality and monitoring as Bangladesh witnessed a five-fold growth in the number of registered private hospitals and clinics since 2000. According to the government's Health Bulletin 2017, the number of registered private hospitals and clinics under DGHS has increased to 5,023 in 2017, which was 3,026 in 2011 and only 1,032 back in 2000. This rapid growth of private sector is a sign of increasing demand and lack of capacity and shortage of health workforce in public sectors. This sector needs to be monitored and regulated properly and the government has to work for increasing its quality.
A large portion of the country's population depends on private medical sector for getting health care services but the government has very little attention for the capacity building as well as monitoring and regulating it. In Bangladesh perspective, private sector occupies a significant portion of health services including clinical care, pharmaceuticals, ambulances, diagnostics, consultancy and so one. A research conducted by icddr,b between 2013 and 2014 on the urban regions found the private sector has lots of challenges and problems such as lack of appropriate law enforcement and regulations, absence of skilled fulltime doctors and nurses, lack of quality care with very limited treatment period along with excessive cost. It also showed that the doctors usually do dual practices that mean government hospitals' doctors checkup patients privately in the afternoon and on the other side the private hospitals do not get efficient nurses as they typically are transferred to government jobs. Some ways to improve the private services can be - introducing accreditation of the sector by the government as a contributing body, improving its quality by strengthening regulations with participatory monitoring, building its capacity and resource with government training and equipment facilities.
By the government's own admission, although funding for healthcare has increased, its total share in healthcare expenditure has been on the decline. In fact it has declined from 37 percent to 23 percent in 2015 and there is massive discrepancy in district-wise allocation of funds with the capital city consuming nearly half the total budget (46 percent). The out-of-pocket experience by our citizens is easy to understand when we see that public health finance amounted to Tk 10,200 crore in 2015 while citizens dished out nearly three times that much (Tk 30,200). What has changed over the years is the rise of private-sector driven healthcare. But going to the doctor nowadays almost always entails pathological tests for even the most rudimentary of ailments like fever and the overzealous prescribing of medication. Patients often are made to go for pathological tests diagnostic centres at doctors' diktat and who does not know in the society that the doctors get part of the exorbitant test fees as bribe money. In public sector, a disproportionate amount of the healthcare budget is being spent on medicines, healthcare services and curative healthcare (71.9 percent). That leaves a paltry 10 percent for investing in preventive healthcare and a measly two percent for education and medical personnel.
As government is not contributing much in providing health services to its people and patients are made to bear two-thirds of the total healthcare costs, the government at least needs to keep a proper monitoring in place, take steps to break the nexus that exists among healthcare practitioners, the pharmaceutical industry and the pathological test centres. There are enormous profits being made at the cost of the people and it is time authorities did something about it. It was outrageous on the parts of private clinics, hospitals and diagnostic centres in Chattogram to go for a wildcat strike and deprive patients of their services for 20 long hours in response to the authorities' drives against rule-flouting medicare institutions at the aftermath of Rafia's death. Such anarchy took place because of a long legacy of lax monitoring and non-enforcement of laws on non-complying private sector operators.
Reaz Ahmad is Executive Editor, United News of Bangladesh


















Leave a Comment
Recent Posts
Populism strikes again
So it is official now - the Bangladesh national team will not be trave ...
Beijing urges Washington to fo ...
China on Thursday reacted to China-related remarks by the US Ambassado ...
The European Union and the Mercosur bloc of South Am ..
New US Ambassador to Bangladesh raises concern over ..
Gold prices in Bangladesh surged past the Tk 250,000 ..
What is Trump's 'Board of Peace' and who will govern ..