Reportage

Two members of the Bangladesh women's cricket team, which remains in quarantine since returning from Zimbabwe amid the Omicron scare late last month, were confirmed last Saturday (December 11) as the country's first identified cases of the latest coronavirus variant of concern.
Since first being identified by South African doctors in the province of Gauteng, which includes Johannesburg in mid-November, Omicron has spread quickly around the globe, and was said to be present in at least 57 countries by the WHO as of December 9 - before Bangladesh confirmed its cases.
Africa recorded more than 107 000 cases in the week ending on 5 December, up from around 55 000, according to WHO - up 93% over the previous week. Countries in southern Africa, where the variant is known to have been in circulation since early November, recorded the highest increase with a 140% hike mainly driven by an uptick in South Africa.
Scientists around the world are poring over the early data out of SA in order to gain a grasp of what to expect in the event of a new wave of infections driven by Omicron. At this stage, the weight of evidence indicates although an Omicron wave may well be inevitable, it is likely to be typified by milder cases, with less severe disease than what was witnessed during the Delta wave.
Data which looked at hospitalisations across South Africa between 14 November and 4 December found that ICU occupancy was only 6.3% - which the WHO says is "very low" compared with the same early period of the wave linked to the Delta variant in July.
Out of more than 1200 admissions, 98 were receiving supplemental oxygen and only four were on ventilation. Most of the people admitted to the health facilities were under the age of 40 - this isn't unusual, as the early part of a wave is often fuelled by the young, who tend to be more outgoing, as well as less vaccinated.
WHO has warned that as the clinical profile of patients changes, the impact of Omicron may change. This would apply even more in countries with a different demographic profile to South Africa, which has a very young population.
But we found some reassuring similarities between the demographic profiles of South Africa and Bangladesh, and even the proportion of the population in each country vaccinated, which makes a deep dive into the early data out of South Africa much more worthwhile.
Similarities between SA and BD
Statistics South Africa, which is a government agency, estimated the population of South Africa was 58.8 million in 2019. In this regard it is dwarfed by Bangladesh, where the population in 2019 was 164.6 million, as per the Bangladesh Bureau of Statistics. But there the dissimilarities end.
According to the World Population Review, which uses projections of the latest United Nations data, the median age in the two countries is very similar - 27.1 in South Africa (26.9 for males, 27. 3 for females), and 26.7 in Bangladesh (26 for males, 27.3 for females).
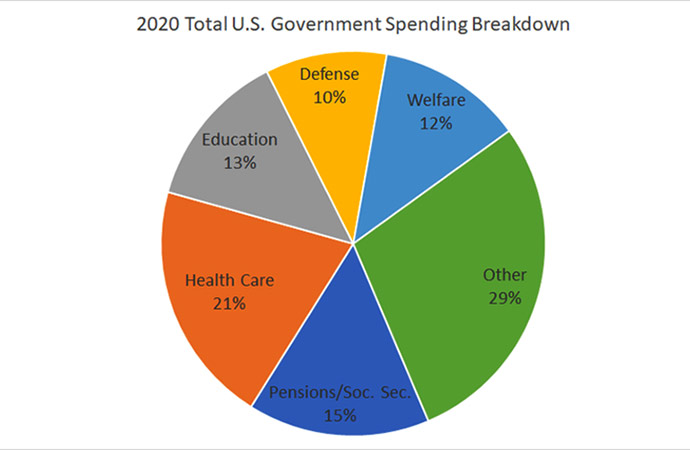
The two countries also have very similar population pyramids (see image), showing the distribution of the population through different age groups. Using World Bank data, we find there are similarities in the age structures of the two nations too.
In South Africa, 28.8% of the population is aged between 0-14 years; 65.6% is aged between 15-64; and 5.5% are 65 and over.
In Bangladesh, 26.8% of the population falls in the 0-14 years category; 68% are between 15-64; and 5.2% are 65 and over.
There are striking similarities in the vaccination numbers too. In South Africa, 41% of the adult population has had at least one dose of the vaccine. In Bangladesh, a greater percentage of the population targeted for vaccination (which includes adults plus some other groups such as students) has had at least a single dose - 52%.
South Africa however has done a better job of fully vaccinating its adult population - 36% are double-jabbed. In Bangladesh, 32% of the targeted population have had their two doses of the vaccine.
South Africa's Fourth Wave
In order to assess the situation in South Africa, we'll look at data from the country's National Institute of Communicable Diseases (NICD), a division of the country's National Health Laboratory Service, hospital groups, and statements of senior healthcare professionals.
The first thing to note is that cases in South Africa are undoubtedly surging. The country confirmed 22,391 new cases on Thursday, 19,018 on Friday, and 17,154 on Saturday, up from about 200 per day a few weeks ago - interestingly, about the level Bangladesh finds itself at present.
The positivity rate hit 29.8% on Thursday, a sharp increase from 1.2% reported during the first week of November.
The new surge has infected 90,000 people in the past month, Minister of Health Joe Phaahla said Friday.
"Omicron has driven the resurgence," Phaahla said, citing studies that say 70% of the new cases nationwide are from omicron.
The R value, signifying the coronavirus reproduction rate - the number of people likely to be infected by one person - for South Africa's current wave is 2.5, which is very high, and the highest that South Africa has recorded during the pandemic.
All this is indicative that Omicron is highly transmissible, probably the most transmissible variant of the virus so far, and a fair bet to replace Delta as the dominant strain worldwide in a matter of weeks.
While clearly well on its way to doing that in South Africa, in the past few days European and UK officials have voiced that expectation too, for their respective jurisdictions.
Waasila Jassat, who tracks hospital data for the National Institute for Communicable Diseases, told the Associated Press that of the patients hospitalized in the current wave, 86% weren't vaccinated against the coronavirus, meaning Omicron, which is notable for its high number of mutations, is able to achieve vaccine escape.
The good news is that doctors and medical experts in South Africa suspect that Omicron really is causing milder COVID-19 than delta, even if it seems to be spreading faster.
According to the NICD, only about 30% of those hospitalised with COVID-19 in recent weeks have been seriously ill, less than half the rate as during the first weeks of previous pandemic waves.
Also according to the NICD, average hospital stays for COVID-19 have shortened significantly, to just 2.8 days in the current wave compared to 8.5 in previous ones.
Jassat said that even though the early signs are that omicron cases are less severe, the volume of new COVID-19 cases may still overwhelm South Africa's hospitals and result in a higher number of severe symptoms and deaths.
Which is where a statement from the CEO of one of South Africa's leading hospital groups comes.
According to Dr Richard Friedland, CEO of Netcare, early trends from the group's hospitals show a "possible decoupling of community transmission rate from hospital admissions."
This means the tendency of hospital admissions to increase in line with the rate of community transmission (or simply the number of people testing positive) may no longer apply. So even if cases rise exponentially, it may not lead to the burden on healthcare systems feared by Wasila Jassat.
In his statement released on Thursday, Dr Friedland noted that in the first three waves of the pandemic (South Africa counts three previous waves, compared to most countries' two), Netcare treated 126,000 COVID-19 patients at its 49 acute care hospitals, of which 55,000 (44%) required hospitalisation and 26% of those patients. were treated in intensive care.
The high admission rate, as well as the high percentage of patients requiring intensive care or intensive care, is indicative of the severity of cases in the first three waves. In the current wave:
"To date, we have 337 COVID-19 positive patients admitted (72% of these patients are in the Gauteng region and 18% in KwaZulu-Natal). Of these patients, approximately 10% (33 patients) are in some form of oxygenation compared to 100% during the first three waves. Eight of those patients (2%) are ventilated and among them two are primary trauma cases who are also positive for COVID-19," Friedland said.
He also said that currently, 90% of COVID-19 cases in Netcare hospitals are considered 'incidental' - i.e. they were admitted for other primary diagnoses or surgical procedures but also tested positive for COVID-19, as Netcare is testing all its patients.
"In the first three waves, when the overall community positivity rate reached 26% in South Africa (remember the recent rates above?), we were inundated with COVID-19 hospital admissions. At Netcare, we had over 2,000 COVID-19 patients in hospitals during the first wave, over 2,250 patients in the hospital during the second wave and over 3,000 patients in the hospital during the third wave. Right now, the 337 patients are a fraction of the previous waves." Friedland added.
"There appears to be a decoupling in terms of the rate of hospital admissions at this early stage of the Fourth Wave."
Public health officials around the world would be praying that holds true. As the NICD's Dr Jassat rightly let on, it has been COVID-19's incredible ability to overwhelm healthcare systems - by making an enormous number of people sick enough to merit hospital admission - that has made it the greatest killer in modern times. If that can be avoided, it leaves the world, including Bangladesh, much better placed to see it through to the finish line of the pandemic, which seemed closer and closer even just six weeks ago.
A decisive decoupling?
Dr Friedland's hunch based on Netcare data is borne out by the NICD's data nationally. They show only a slight increase in the number of overall hospitalisations from the start of November till date, but the rate of hospital admissions (percentage of active cases hospitalised) has plunged dramatically - even as cases have surged on the back of Omicron.
On November 1, South Africa had some 18,600 active cases, of whom 3838 were hospitalised - over 20%. Today there are over 149,500 active cases in South Africa, but just 3.6% of them are hospitalised - some 5400. Almost any country in the world would take that.
Over the past few weeks, a number of South African doctors, while cautioning that it will take many more weeks to collect enough data to be sure, and to always take Covid-19 very seriously and to be as careful as ever, have come out and expressed their optimism over Omicron. But in amid all the hysteria, their voices have often been drowned out.
There was Dr. Angelique Coetzee, a private practitioner and chair of the South African Medical Association, who was the first to spot the variant and also the first to report its 'extremely mild' symptoms. She said unlike the Delta, her patients early on had not reported loss of smell or taste and there had been no major drop in oxygen levels with the new variant.
"The most predominant clinical complaint is severe fatigue for one or two days. With them, the headache and the body aches and pain," Dr Coetzee reported.
Dr. Unben Pillay, a practitioner in Gauteng, told AP he is seeing dozens of sick patients a day. Yet he hasn't had to send anyone to the hospital.
"They are able to manage the disease at home," Pillay said of his patients. "Most have recovered within the 10 to 14-day isolation period."
And that includes older patients and those with health problems that can make them more vulnerable to becoming severely ill from a coronavirus infection, he said.
Over the next few weeks, we may witness case numbers jump in Bangladesh, as the highly transmissible Omicron variant spreads in Bangladesh. For now, Health Minister Zahid Maleque has said there is no reason to believe the virus has spread from the two infected cricketers.
"Both the players are doing well. There is no reason to worry about the Omicron variant," the minister said while addressing an event at Dhaka Medical College Hospital this afternoon.
South Africa, which has been slapped with travel bans, is said to have been 'punished for excellent science' in picking up and identifying the new variant so quickly. Its case numbers are also a reflection of its extensive testing regime.
One possibility is that due to Bangladesh's far less rigorous testing protocol, the country experiences an almost invisible wave, in which the vast majority of people who pick up the virus are not even tested, due to a lack of symptoms. Yet through this wave, the country attains a level of herd immunity, and crosses the threshold at which COVID-19 stops being an epidemic, and enters the endemic stage.
The next few weeks will be telling.


















Leave a Comment
Recent Posts
Right On Schedule
The most eagerly anticipated, and frankly hyped up, announcement of an ...
Fighting raged along the borde ...
Fighting raged along the border of Cambodia and Thailand, with explosi ...
ICIMOD drives regional cooperation to inspire new mo ..
The Cage of Captivity and the Cry for Freedom: A Cru ..
Why Japan issued an advisory for a possible megaquak ..
The Autocrats’ War on Universities