Reportage

Photo: UNB
Dhaka Medical College Hospital (DMCH), one of Bangladesh's largest public healthcare facilities, is facing a severe crisis as mismanagement and overcrowding jeopardise patient care.
With patient numbers nearly double the intended capacity, the hospital is struggling to provide adequate services, exposing critical issues that burden patients and their families.
Upon entry, visitors are met with unsanitary conditions, insufficient food provisions, and inadequate staffing.
Many patients are seen lying on the floors of overcrowded corridors and wards, underscoring the scale of the crisis.
Brigadier General Asaduzzaman Khan, the hospital's director, has acknowledged the growing complaints and pledged to address these ongoing issues.
Patients Endure Delays and Lack of Medical Supplies
Alal Uddin, who suffered a head injury in an accident in Mymensingh, had been waiting in the corridor since 4 October, unable to secure a bed.
His brother, Jalal Uddin, voiced frustration, saying, "Nurses are unavailable when needed, and doctors are also hard to reach."
Another patient, 24-year-old Jahid Hasan, admitted on October 2, had faced similar challenges. His father, a CNG driver from Khilgaon, revealed, "A prescribed injection has not been administered as it's reportedly out of stock, despite being listed in the hospital pharmacy."
Many families are forced to purchase medicines externally due to shortages at the hospital.
Lack of Hygiene Raises Health Concerns
Hospital staff struggle to maintain hygiene standards amidst overcrowding.
The director cited users' behaviour as a factor, explaining, "Toilets are often misused, with discarded items blocking the facilities. With each toilet shared by around ten people, maintaining proper sanitation becomes difficult."
A visit to the hospital kitchen revealed further issues, including waste accumulation near cooking areas and rice left uncovered, raising health concerns for patients.
Understaffing and Financial Constraints
A shortage of class four staff exacerbates the situation, according to the director. "Without increasing personnel, mismanagement will continue."
Besides, the daily food budget of Tk 150 per patient is inadequate, he added, advocating for an increase to Tk 200 for improved meal quality.
Corruption Allegations Add Financial Strain
Some patients and families report being asked to pay tips of Tk 50-100 to hospital aides for basic services such as wheelchair assistance.
A ward aide, speaking on condition of anonymity, explained, "If patients offer us something, it helps us manage our own expenses."
The director acknowledged the issue, noting, "We have dismissed individuals involved in such practices, though eradicating it entirely remains a challenge."
Improving Bangladesh's Healthcare System
Experts call for reforms to improve Bangladesh's healthcare, including stricter regulations for private clinics, decentralised recruitment for healthcare professionals, and a more equitable doctor-patient ratio. Other challenges include unregulated pharmacies, reactive health-seeking behaviour, and high out-of-pocket costs for patients.
A Legacy Under Strain
Founded in 1946, Dhaka Medical College has evolved over decades, with expansions that include a new complex opened in 2013. However, demand consistently outstrips capacity.
With 39 public and 68 private medical colleges nationwide, the country still struggles to meet the healthcare needs of its population.
At the heart of hospital management is the commitment to quality patient care, according to experts. They said that this involves not just medical treatment, but also ensuring patient safety, privacy, and satisfaction.
Hospitals must continuously monitor and improve their care processes to meet the highest standards.
The rising cost of healthcare in Bangladesh poses a serious challenge for the general public, many of whom rely on government hospitals for affordable services.
Dhaka Medical College Hospital (DMCH), along with facilities like Suhrawardy Hospital and the Dhaka Children's Hospital, is often the first line of care for a population that cannot afford private treatment.
Yet despite offering lower-cost services, these hospitals frequently leave patients dissatisfied, prompting them to seek alternative options in private hospitals despite the financial strain.
Resource Constraints in Public Hospitals
Brigadier General Asaduzzaman Khan, Director of DMCH, openly acknowledges the difficulties faced by public healthcare facilities, citing high patient volumes and limited resources as significant hurdles.
"Demand far exceeds our capacity," he said, noting that public hospitals like DMCH operate under considerable pressure, leading to overcrowding, long wait times, and shortages of essential resources.
With a population largely reliant on these services, patients are often forced to endure cramped wards, extended delays, and varying levels of staff engagement.
The impact of these conditions on patients is profound.
Milon Haque, a small business owner admitted to DMCH, shared his experience of inadequate care due to the overwhelming number of patients. "I had several health complications, but I couldn't get timely attention from the doctors," he explained, describing not only the delays but also the poor facilities and unprofessional conduct of certain staff members.
The lack of proper care ultimately drove him to seek treatment at a private clinic, stretching his limited budget.
For Milon, private care is a considerable financial burden, but one he feels compelled to bear given the circumstances.
This story resonates with many, particularly parents with young children who seek treatment at Dhaka Children's Hospital.
A couple recently took their two-year-old daughter, Mahi, there, only to leave in search of a private hospital when they could not secure a bed.
"I don't know how long we can bear the expense, but my child's health is my priority," Mahi's father explained. This desperate choice between personal finances and essential care is one that many families face when navigating the public healthcare system.
Appeal of Private Healthcare
Private hospitals, while expensive, offer a contrasting experience that attracts those willing to make financial sacrifices. Patients generally report higher satisfaction with the quality of private hospital services and facilities, even though these options come at a steep price.
Enamul Karim, 58, recently received treatment at a private hospital and described it as a positive experience, noting that it felt vastly different from the challenges he encountered in public hospitals.
"Doctors in government hospitals are incredibly skilled, but due to the volume of patients, we often miss out on direct services. Many of them have private practices, and while expensive, it's often preferable to go there," Enamul explained.
This sentiment is echoed across various socio-economic backgrounds. For many, the decision to choose private care stems from a need for reliable and timely attention that government hospitals, under pressure to serve large numbers of people, struggle to provide.
Rising Out-of-Pocket Expenditures
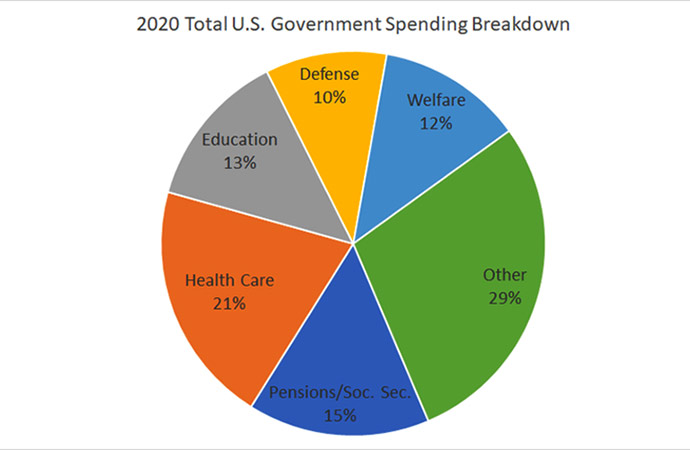
The Directorate General of Health Services' Health Economics Unit reports a troubling trend: out-of-pocket health expenditure has surged to around 69 percent in Bangladesh as of 2020.
Pharmaceuticals constitute a significant portion of these expenses, followed by diagnostics and other medical services.
The general economic downturn and rising cost of living have only exacerbated the situation, making healthcare unaffordable for many.
Public health experts are alarmed by this rising expenditure, which forces individuals to choose between financial security and essential health services. Delaying care due to financial concerns can lead to worsened health conditions and higher long-term treatment costs.
Besides, "out-of-pocket health expenses" encompass non-medical costs that impact productivity, lost wages, and transportation expenses, which, though often overlooked, place a heavy burden on individuals and families alike.
Health economics research categorises these expenses into three groups: direct medical (costs of healthcare resources), direct non-medical (costs like transportation and caregiver support), and indirect (lost productivity).
These expenses cumulatively create an enormous economic burden that impacts families and the wider society. Comprehensive evaluations of healthcare costs, including non-medical expenses, are essential to understanding the true financial impact of the current system.
Structural Inequities in Bangladesh's Healthcare System
Bangladesh's healthcare infrastructure encompasses over 3,976 public facilities and 975 private hospitals and clinics.
Yet, despite this extensive network, public healthcare usage remains low due to system inefficiencies and lack of resources. Research by the Centre for International Epidemiological Training (CIET) found that only 13% of Bangladeshis use government services, while 27% turn to private or NGO services.
Alarmingly, a large majority - 60% - resort to unqualified providers due to accessibility and affordability concerns.
A study led by Syed Saad Andaleeb of Pennsylvania State University suggests that the economic framework within which these hospitals operate impacts service quality.
Public hospitals operate under constrained government budgets, whereas private hospitals are incentivised by client fees, motivating them to provide higher-quality care to attract and retain patients.
This dynamic results in a significant disparity, pushing many people to seek out private facilities despite the cost.
A Growing Call for Healthcare Reform
The stories emerging from DMCH and similar institutions underscore the urgent need for systemic reform.
Addressing the barriers to quality care requires strategic shifts in resource allocation, improvements in patient management, and enhanced staff training within public healthcare facilities.
Policymakers and healthcare professionals are increasingly calling for reforms to bridge the gap between public and private healthcare services, easing the financial strain on patients while providing accessible, quality care.
Efforts to address out-of-pocket expenses and promote affordable healthcare align with the goals of the "Health Care Financing Strategy 2012-32."
This strategy envisions a healthcare system where financial constraints do not dictate access to quality medical treatment. With the right reforms, Bangladesh can make strides toward this goal, ensuring that affordable healthcare becomes a reality for its citizens.
As Bangladesh moves forward on its development journey, the stories of individuals like Milon and Mahi's family highlight a pressing challenge: securing accessible, high-quality healthcare for all.
Public hospitals like DMCH, the backbone of the national healthcare system, play a vital role in this endeavour.




















Leave a Comment
Recent Posts
Auspicious beginnings, but a l ...
The newly elected government of Bangladesh is now in office, and the e ...
Caught between tigers and pira ...
Over 10,000 fishermen in the Sundarbans have suspended their fishing a ...
Historic Chawk Bazar comes alive with iftar items on ..
Shaping Young Conservationists: School Conservation ..
Iran has said it has reached an understanding with t ..
New Finance Minister Amir Khosru Mahmud Chowdhury